Note: This is an automated translation (using DeepL) of the original German article.
EMS-Data shows: Vaccination offers reliable protection, also against infection with Delta variant
The protective effect of the Corona vaccination is regularly questioned or even denied. Currently, the increasing number of vaccine breakthroughs is used as an argument for this.
Why this argumentation is not true, we want to illuminate in three steps:
- These claims can be refuted with simple considerations.
- the comparison of vaccinated and unvaccinated persons, as well as the infections of vaccinated and unvaccinated persons, shows that vaccination is effective.
- Finally, with the help of data from the Epidemiological Reporting System (EMS), the vaccination effectiveness can be calculated. It is 78.5% in Austria, based on EMS data (for mRNA vaccines, see [5] at Annotations & Limitations).
Graph 1 shows the impact of a vaccine efficacy of 78.5% on the incidence of infection. While 3,074 people tested Covid positive out of every 100,000 unvaccinated, only 662 did so in the vaccinated group. So vaccinated people have a much lower risk.
In the following, we will go through the three points step by step and see that the vaccine efficacy also applies to the delta variant.
Before that, however, we briefly review the necessary definitions and data basis.
{< dwhadddiv “lalalala” >}}
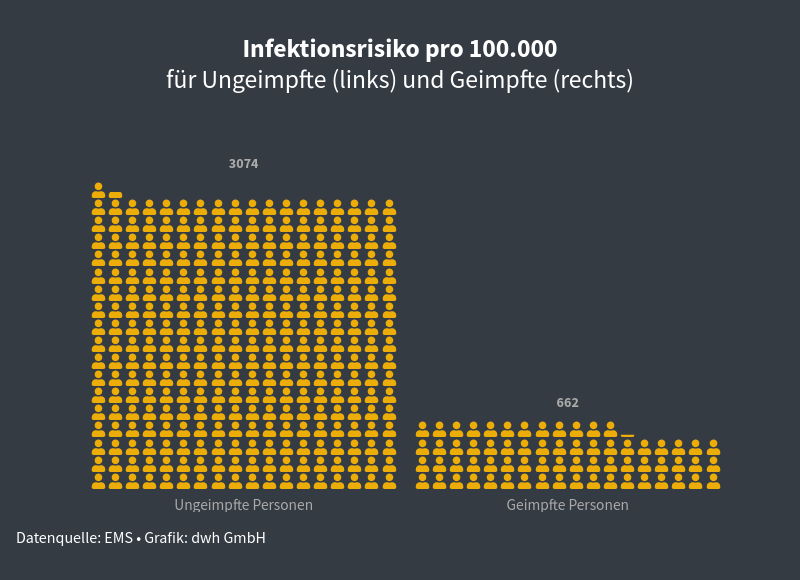 .
Graph 1, left: During the observation period [4] of every 100,000 unvaccinated individuals 3,074 became infected with Covid-19. Right: thanks to vaccine efficacy of 78.5%, only 662 people became infected out of every 100,000 vaccinated people during the same period.
.
Graph 1, left: During the observation period [4] of every 100,000 unvaccinated individuals 3,074 became infected with Covid-19. Right: thanks to vaccine efficacy of 78.5%, only 662 people became infected out of every 100,000 vaccinated people during the same period.
Definitions and data situation
The Robert Koch Institute (Germany) defines vaccine breakthrough, “when a PCR-confirmed SARS-CoV-2 infection with symptomatology is detected in a fully vaccinated person. “ More than 14 days must have elapsed since the “last required vaccine dose” (see [1] at Notes & Limitations).
Thus, for an analysis, the vaccination data (who was vaccinated and when) plus data on the severity of the disease (asymptomatic or symptomatic or even hospitalized) are needed. In Austria, the Epidemiological Reporting System (EMS) registers all confirmed Covid-19 cases (positive PCR test), but “without” severity of illness (see [2]). Therefore, the system does not distinguish between infected persons without symptoms and diseased persons with symptoms. Therefore, the number of vaccine breakthroughs (as defined above) cannot be calculated with these data.
However, it is possible to calculate how many people with and without vaccination tested positive, i.e., became infected (see [3]). This number includes the symptomless and is therefore higher than the symptomatic alone. On the other hand, there is also a risk of test bias by which fewer infections are detected among vaccinated individuals (test bias; see [7]). Overall, however, an estimate is obtained for the effectiveness of vaccination.
1) More vaccinations mean more covid cases among vaccinated individuals.
The following simple consideration is helpful for basic understanding:
- one year ago, in November 2020, there was no Corona vaccination. At that time, therefore, every Corona case detected (logged in the EMS) is an unvaccinated person. Vaccine breakthroughs or infections of vaccinated individuals are therefore not possible. 2 Assume, on the other hand, that a population consists of only (more) vaccinated persons. This corresponds to a vaccination coverage rate of 100% and is the reverse of the situation one year ago. In this population, every covid infection affects one vaccinated person.
- Thus, if we look at the number of vaccine breakthroughs alone, they clearly increase with the number of vaccinated persons in the total population.
Since no vaccination offers 100% protection, there is a residual risk of falling ill even for vaccinated persons - until eradication of a disease (as was achieved with smallpox, for example). This risk is greater the more widespread the disease is in the population. Austria has a vaccination coverage rate of 66% of the total population (fully vaccinated) and covid case numbers have been rising for weeks (as of 11/22/2021). So it is obvious that the number of infections among vaccinated people is also increasing.
Much more essential than this (absolute) number of infections among vaccinated persons is therefore the question: what difference does vaccination make? Or asked differently: Does vaccination work at all, and if so, how well?
2) The effectiveness of the vaccination …
And this question is where it gets interesting. Because here the situation is not immediately obvious - as we will see.
Note: For simplicity, we refer to persons without a completed vaccination series as “unvaccinated persons”. “Vaccinated persons” are, conversely, those with completed vaccination series (see [1]).
To this end, we first consider the number of confirmed infections among unvaccinated and among vaccinated persons. In Austria, 5.5 million people are vaccinated and 3.4 million are not. Thus, there are approximately twice as many vaccinated people (green) as unvaccinated (blue), as shown in the graph (left side). (As of 10/31/2021, see [4]).
During the observation period, 146,979 Covid-19 infections were reported in Austria. Of these, 42,287 cases affected vaccinated individuals, while the large remainder of illnesses (104,692 cases) affected unvaccinated individuals (right graph).
Thus, although nearly twice as many people were vaccinated, nearly 3/4 - the vast majority - of all reported cases affected unvaccinated persons*! So vaccination is working. Exactly how well can be calculated with the EMS numbers.
3) … calculated with real numbers.
Vaccination protection depends on the vaccinated agent. For simplicity (see [5] & [8]), we consider below only the two mRNA vaccines (Pfizer/BioNTech and Moderna). These two have very similar efficacy. They are also the most frequently vaccinated in Austria: nearly half (49.9%) of all Austrians are vaccinated with them (see Table 1, as of 10/31/2021). Together, these two vaccines account for 80% of all vaccinations.
| population total | unvaccinated | vaccinated total | vaccinated with mRNA | |
|---|---|---|---|---|
| Absolute | 8,932,664 | 3,406,237 | 5,526,427 | 4,458,920 |
| Percentage | 100% | 38.1% | 61.9% | 49.9% |
Table 1: Population in Austria by vaccination status, as of 31.10.2021, source: EMS.
Vaccination effectiveness is the difference between infections of vaccinated persons compared to unvaccinated persons. Or, more specifically, the ratio of the infection rate among the vaccinated to the infection rate among the unvaccinated.
We therefore need the infection figures for the observation period from September 1 to October 31, 2021, which can be found in Table 2. For the sake of completeness, all infections nationwide (total) are listed, as well as those for vaccinated persons with all vaccines.
| Total | Unvaccinated | mRNA vaccinated | (all vaccines) | |
|---|---|---|---|---|
| humans | 8,932,664 | 3,406,237 | 4,458,920 | (5,526,427) |
| Infected | (146,979) | 104,692 | 29,536 | (42,287) |
| infected in % | (1.65%) | 3.07% | 0.66% | (0.77%) |
| and per 100,000 | (1645) | 3074 | 662 | (765) |
Table 2: New infections by vaccination status in Austria in the observation period: 1.9.-31.10.2021, source: EMS.
During this period, 3.07% of the unvaccinated population became infected with Covid-19 and 0.66% of those vaccinated with mRNA vaccine. Percentages denote risk of infection per 100 persons. Thus, for the unvaccinated, the risk of becoming infected is 3.07 : 0.66 = 4.65 times greater than for the vaccinated. (In percent: The risk is 465% higher for the unvaccinated! Conversely, the risk with vaccination is 0.66 : 3.07 = 0.215 less than without vaccination. This corresponds to 21.5%.
If the risk of getting sick without vaccination is our standard (100%), and vaccination reduces the risk to 21.5%, then vaccination has an effectiveness of 100% - 21.5% = 78.5%. And this is exactly how vaccine efficacy is calculated:
$$vaccine efficacy = 1 - {infection_rate_{vaccinated} {infection_rate_{unvaccinated}}.$$
In our case, with the mRNA infection rate of 0.66% and that among unvaccinated of 3.07% (see Table 2), this results in.
$$vaccine efficacy = 1 - {0.66 \over 3.07} = 78.50 \mathrlap{\it{/}}{^0}_{0}.$$
Therefore, the vaccine protection calculated from the real case numbers in Austria is 78.5% (for the two mRNA vaccines). During the observation period, the delta variant was already the dominant variant. Vaccination therefore also provides very reliable protection against the delta variant. Moreover, this vaccine efficacy refers to all cases registered in the EMS. That is, even taking into account all asymptomatic cases and those with only mild symptoms, there is an excellent vaccine protection [7].
To illustrate this graphically, here again is graph 1 from the beginning:
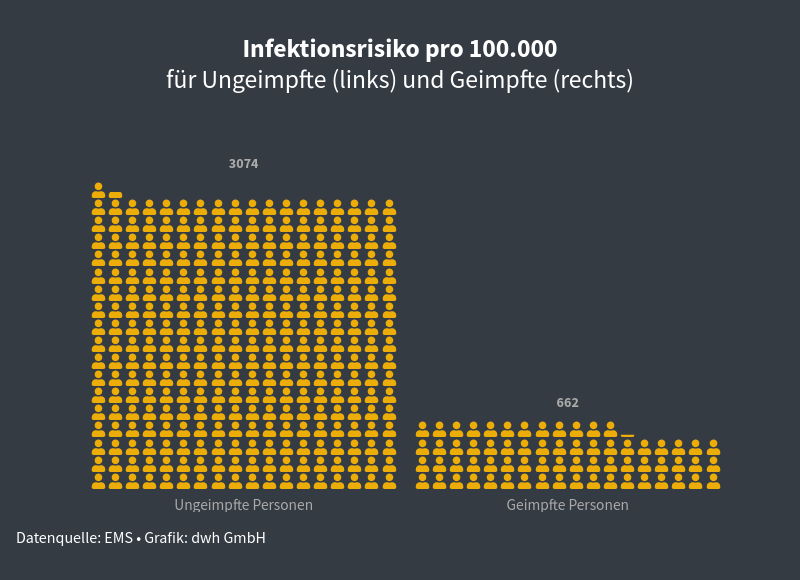 .
Graph 1, left: During the observation period [4] of every 100,000 unvaccinated individuals 3,074 became infected with Covid-19. Right: thanks to vaccine efficacy of 78.5%, only 662 people became infected out of every 100,000 vaccinated people during the same period.
.
Graph 1, left: During the observation period [4] of every 100,000 unvaccinated individuals 3,074 became infected with Covid-19. Right: thanks to vaccine efficacy of 78.5%, only 662 people became infected out of every 100,000 vaccinated people during the same period.
Annotations & Limitations
- Further information on vaccination recommendations and vaccines can be found on the FAQ page of the Robert Koch Institute.
- In the EMS, a severity level is deposited to some extent. However, this information is not meaningful/accurate enough to make reliable evaluations. However, there is one exception: if the person dies of/with covid this is stored in the system with a relatively good quality. Note: The AGES is trying to collect the severity data (retrospectively), but this information is not included in this evaluation.
- Vaccine efficacy analyses are usually done for efficacy against a) infection, b) symptomatic disease, c) hospitalization, d) requires intensive care, or e) death. In many countries, data are collected for b). For a), systematic PCR screening of predefined groups is necessary (expensive and laborious). The analysis performed here should be seen as an intermediate form of a) and b).
- In order to get meaningful and comparable results, the period 9/1/2021 to 10/31/2021 was used. The reason: within this observation period, on the one hand, the vaccination rate has remained approximately unchanged and, on the other hand, the infection incidence has been very active. The cut-off date for the following data is 31.10.2021.
- In order to keep the detailed analysis manageable and easier to understand, only mRNA vaccines were focused on. The reason for this, besides the difference in efficacy, is that the use and vaccination recommendations have changed significantly for the other two vaccines: De facto stop by AstraZeneca and urgent recommendation for second vaccination by Johnson&Johnson. Therefore, the collection of the necessary data here would also be much more complicated.
- official data on Covid-19 case numbers in hospitals and intensive care units with information on vaccination status in Austria are unfortunately not available (not systematically collected), so we have to make do with EMS data.
- The number of unreported cases is not included in these calculations. Since vaccination protects against (severe) symptoms, it is likely that the underreporting rate among vaccinated persons is higher because an (asymptomatic) infection is not noticed. In addition, a testing bias among vaccinated persons is to be expected, since vaccinated persons may test themselves less often. Reasons for this include lack of need (in 3G regimen) or different contact classification (K2 instead of K1).
- The (additional) effectiveness of booster vaccinations was deliberately not considered in this analysis to keep it easier to understand. It takes 14 days after administration for the booster vaccine to reach nominal efficacy. Allowing for this two-week delay, 197,650 were administered by the end of the observation period (including 10/31/2021). Out of 4,458,920 persons vaccinated with mRNA, this corresponds to a proportion of 4.4%.
